Office of Infectious Disease Epidemiology
Lyme disease is caused by the bacteria Borrelia burgdorferi, named after the scientist who discovered it in 1982 – Willy Burgdorfer. It is spread by the bite of an Ixodes scapularis tick, also known as a blacklegged tick or deer tick.
What are the Symptoms of Lyme Disease?
Lyme disease can cause a variety of symptoms, depending on the stage of infection.
Early Signs and Symptoms (3 to 30 Days After Tick Bite)
- Fever, chills, headache, fatigue, muscle and joint aches, and swollen lymph nodes.
-
Erythema migrans (EM) rash:
- Does NOT occur in all infected persons. It is estimated that 70 to 80 percent of infected persons will develop the EM rash.
- Can appear on any part of the body and is NOT usually itchy or painful.
- The appearance can vary WIDELY. Click this link to view Lyme disease rashes and look-alikes.
The appearance of the EM rash does not always appear as a “classic” bullseye rash. Photo credit: CDC.
Later Signs and Symptoms (Days to Months After Tick Bite)
- Severe headaches and neck stiffness
- Additional EM rashes
- Droop on one side or both sides of the face (facial palsy)
- Arthritis with severe joint pain and swelling, usually on the knees and large joints.
- Heart palpitations or an irregular heartbeat
- Dizziness or shortness of breath
- Nerve pain
- Shooting pains, numbness, or tingling in the hands or feet
How Does Lyme Disease Spread?
The Lyme disease bacterium is spread through the bite of an Ixodes scapularis tick (also known as a blacklegged tick or deer tick). Blacklegged ticks are found in every county of Delaware. Learn more about tick species of Delaware here.
Approximate sizes of Ixodes scapularis ticks. Photo credit: CDC.
Since the blacklegged tick is the only species of tick that can spread Lyme disease in Delaware, it is important to save the tick or take a picture of it for identification. Knowing what species of tick has attached to you, a family member, or a pet will help determine whether you may be at risk for a tick-borne disease.
Found a tick and want to know what species bit you? Report the tick bite to DNREC’s Tick Program by clicking the tick image below:
There is no evidence that Lyme disease is transmitted from person-to-person. For example, a person cannot get infected from touching, kissing, or having sex with a person who has Lyme disease. Pregnant persons should seek treatment as soon as possible since Borrelia burgdorferi can infect the placenta.
It is important to note that a person can get Lyme disease more than once if they are bitten by another infected tick.
Diagnosis
Most Lyme disease tests detect antibodies made by the body in response to infection. The CDC currently recommends a two-step process for Lyme disease antibody testing. If the first test (usually an ELISA test) is negative, no further testing is recommended. If the first test is positive or equivocal, the second test (usually a Western Blot) should be performed. The overall result is positive only when the first test is positive (or equivocal) and the second test is positive (or for some tests equivocal). Antibodies can take several weeks to develop, so patients may test negative if infected only recently. It is important to note that antibodies can persist in the blood for months or even years after the infection is gone, so these tests cannot be used to determine cure.
New modified two-tier tests (MTTTs) were approved by the FDA in 2019. The MTTTs are more sensitive than the standard two-tier tests during the early stages on Lyme disease infection
Treatment
Most cases of Lyme disease can be treated with a few weeks of antibiotics. Depending on symptoms, some patients may require a second course of antibiotic therapy. Patients with certain neurological or cardiac forms of illness may require intravenous (IV) antibiotics. Multi-month prescriptions on antibiotics are not recommended and have not been shown to be effective.
About 5-10% of patients with Lyme disease have sympotoms that last months to years after treatment with antibotics called Post-Trestment Lyme Disease Syndrome (PTLDS). These sympotoms can include muscle and joint pains, arthritis, cognitive defects, sleep disturbance, and fatigue. The cause of these symptoms is not known. Reperated treatments with antibiotics have not been shown to be effective in treating PTLDS. Additional research is needed to better understand how to treat, amanage, and support people with persistent syptoms associated with Lyme disease.
How Many Cases of Lyme disease are There in Delaware?
Lyme disease is the most common vector-borne disease in Delaware. Delaware is considered a high-incidence Lyme disease jurisdiction, which means that the First state had an average Lyme disease incidence of ≥10 cases/100,000 population for a period of three consecutive years. See Lyme disease human cases for more specific data.
Avoiding Tick Bites
- Avoid wooded or brushy areas with high grass and leaf litter.
- Stick to the center of trails.
- Treat clothing with products containing 0.5% permethrin or use EPA-registered insect repellents containing products like DEET. Always follow label instructions.
- Perform tick checks on yourself, children, and pets after being outdoors.
- Shower within two hours of coming indoors and tumble dry clothes in a dryer on high heat for 10 minutes to kill ticks.
- Keep pets up to date on tick preventive products.
Tick Safety at Home
-
Create a “
Tick-Safe Zone”
through landscaping.
- Place a three-feet wide barrier of wood chips or gravel between lawns and wooded areas and around patios and play equipment.
- Maintain a nine-feet wide barrier between the wood chips and high-use areas.
- Remove leaf litter and invasive plants (e.g., multiflora rose, Japanese honeysuckle, Japanese barberry, Oriental bittersweet).
- Keep grass short in high-use areas and keep leaves raked.
- Keep your yard free of trash which may attract rodents.
Education and Outreach
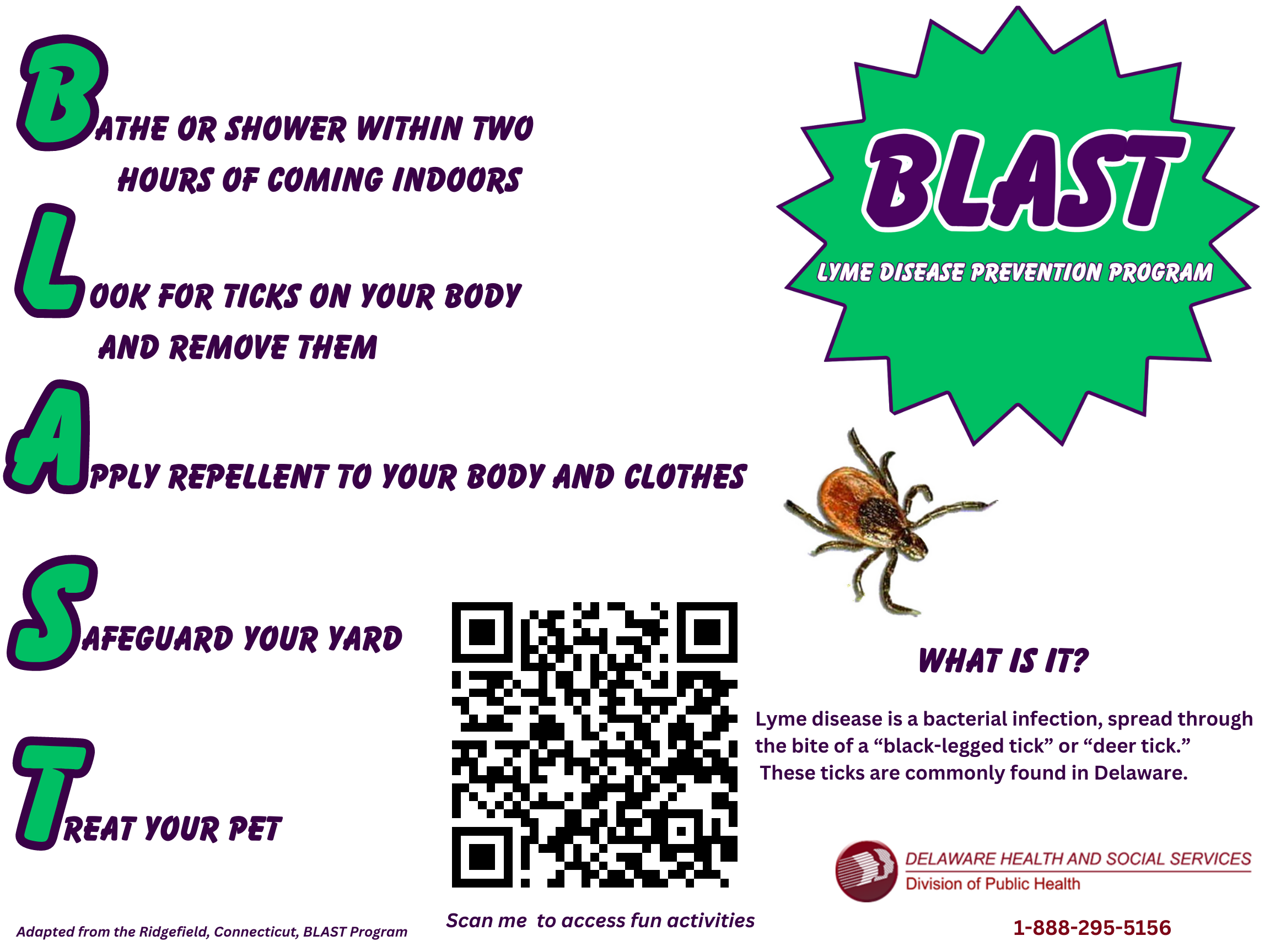
BLAST Program
- The BLAST program was adapted by the Delaware Division of Public Health from the Ridgefield Connecticut program
- Its purpose is to raise awareness on the most effective Lyme disease prevention practices and educate the community about the signs and symptoms of Lyme diseases.
Kids Korner
Office of Infectious Disease Epidemiology
24/7 Emergency Contact Number: 1-888-295-5156
Return to Infectious Disease Home Page
![]() Please note: Some of the files available on this page are in Adobe PDF
format which requires Adobe Acrobat Reader. A free copy of Adobe Acrobat Reader can be downloaded directly from Adobe . If you are using an assistive technology unable to
read Adobe PDF, please either view the corresponding text only version (if available) or visit Adobe’s Accessibility Tools page.
Please note: Some of the files available on this page are in Adobe PDF
format which requires Adobe Acrobat Reader. A free copy of Adobe Acrobat Reader can be downloaded directly from Adobe . If you are using an assistive technology unable to
read Adobe PDF, please either view the corresponding text only version (if available) or visit Adobe’s Accessibility Tools page.